Receptors of the ANS
Usually, a particular receptor subtype for each division of the ANS will dominate in a certain gland or organ. In general, activation of some receptor subtypes leads to stimulation of the effector and activation of others to inhibition of the effector. Even numbered subtypes are usually inhibitory and odd numbered subtypes are usually excitatory, but there are no hard and fast rules. Ultimately, the relative amounts of each receptor subtype expressed in the tissue will determine the overall effect (stimulation or inhibition) on the particular gland or organ. Similar to how neurons can be classified by the neurotransmitter they release, receptors can be classified by the type of neurotransmitter they receive. Cholinergic receptors receive acetylcholine and adrenergic receptors bind to catecholamines. This can get confusing at times because it is possible that a adrenergic neuron (one that releases norepinephrine) will have cholinergic receptors. This would be the case for most of the post ganglionic neurons in the sympathetic nervous system.
Cholinergic Receptors
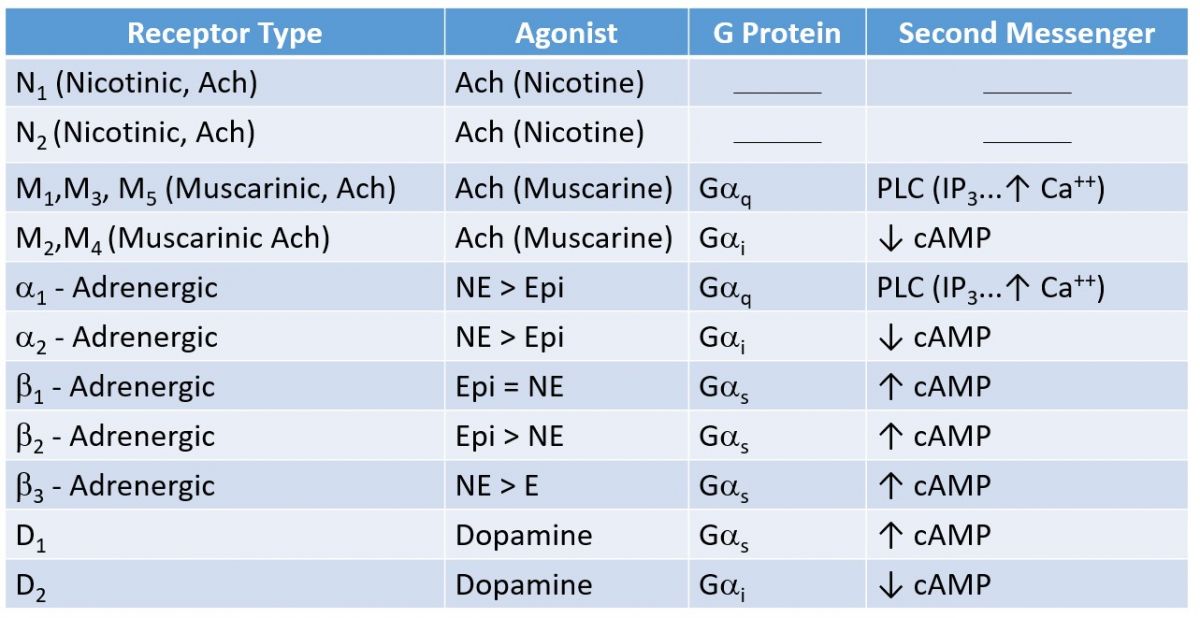
As mentioned, preganglionic neurons of both sympathetic and parasympathetic divisions produce and release ACH. The receptors for ACH are known as cholinergic receptors. There are two main subtypes of cholinergic receptors; nicotinic and muscarinic. They are named after alkaloids found in tobacco and certain mushrooms respectively. The alkaloid nicotine specifically activates nicotinic cholinergic receptors, while muscarin activates muscarinic cholinergic receptors, and ACH activates both types. The cell bodies of postganglionic neurons for both sympathetic and parasympathetic nervous systems express nicotinic receptors (see figure above). To distinguish nicotinic receptors in neurons from nicotinic receptors found in the neuromuscular junction, we use the terms nicotinic (N1 or N2) cholinergic receptors. N1 are located in the neuromuscular junction and N2 are used in the ANS. Similar to the neuromuscular junction, stimulation of nicotinic type II (N2) channels results in the entry of Na+ which depolarizes the post synaptic neuron.
Muscarinic receptors (M) are located on cells of all parasympathetic effectors and on cells of some sweat glands innervated by the sympathetic nervous system. There are several subtypes of muscarinic receptors (M1-M5) which may be stimulatory (depolarization) or inhibitory (hyperpolarization)
Adrenergic Receptors
As mentioned, neurons that produce and release the neurotransmitter NE are known as adrenergic neurons. NE is secreted by postganglionic neurons of the sympathetic nervous system and binds to adrenergic receptors expressed on effector cells. Epinephrine (EPI) released by the adrenal gland also binds to adrenergic receptors expressed on effectors (see figure above). There are two main types of adrenergic receptors, namely, alpha and beta which have several subtypes. For our purposes, we will focus on the following five subtypes: alpha 1, 2, and beta 1, 2, and 3. Activation of adrenergic receptors expressed on effectors by NE or EPI may result in stimulation or inhibition of the effector depending on the tissue involved. Odd subtypes of adrenergic receptors (alpha 1, and beta 1, and 3) generally have stimulatory effects and even subtypes (alpha 2 and beta 2) have inhibitory effects. NE has a stronger affinity for alpha 1 receptors than EPI and EPI has a stronger affinity for Beta-2 receptors than NE. Below is a table that summarizes the receptor types and the second messenger system involved with stimulation of that receptor.